Eating disorders are often associated with physical changes—weight loss, fatigue, hormonal disruptions—but the impact extends beyond the body. Anorexia nervosa in particular affects the brain in significant and often misunderstood ways. These neurological changes can influence everything from mood and memory to decision-making and emotional regulation. They help explain why recovery is so challenging, even when someone wants to get better.
For loved ones and care providers, recognizing the brain-based nature of anorexia can foster greater patience, reduce misplaced blame, and support more effective treatment approaches.
1. It Disrupts Brain Chemistry Through Malnutrition
Food is not just fuel for the body. It is essential to the brain’s chemical balance. When someone consistently under-eats, the body lacks the nutrients required to produce key neurotransmitters, including serotonin. Without adequate carbohydrates and proteins, serotonin synthesis slows, affecting mood regulation, digestion, and sleep.
Low serotonin levels are associated with heightened anxiety, depressive symptoms, obsessive thinking, and gastroparesis (a slowing of digestion). In those with anorexia, this can create a feedback loop: restrictive eating alters gut function and mental state, which in turn reinforces the urge to restrict.
2. It Interferes With Reward Pathways
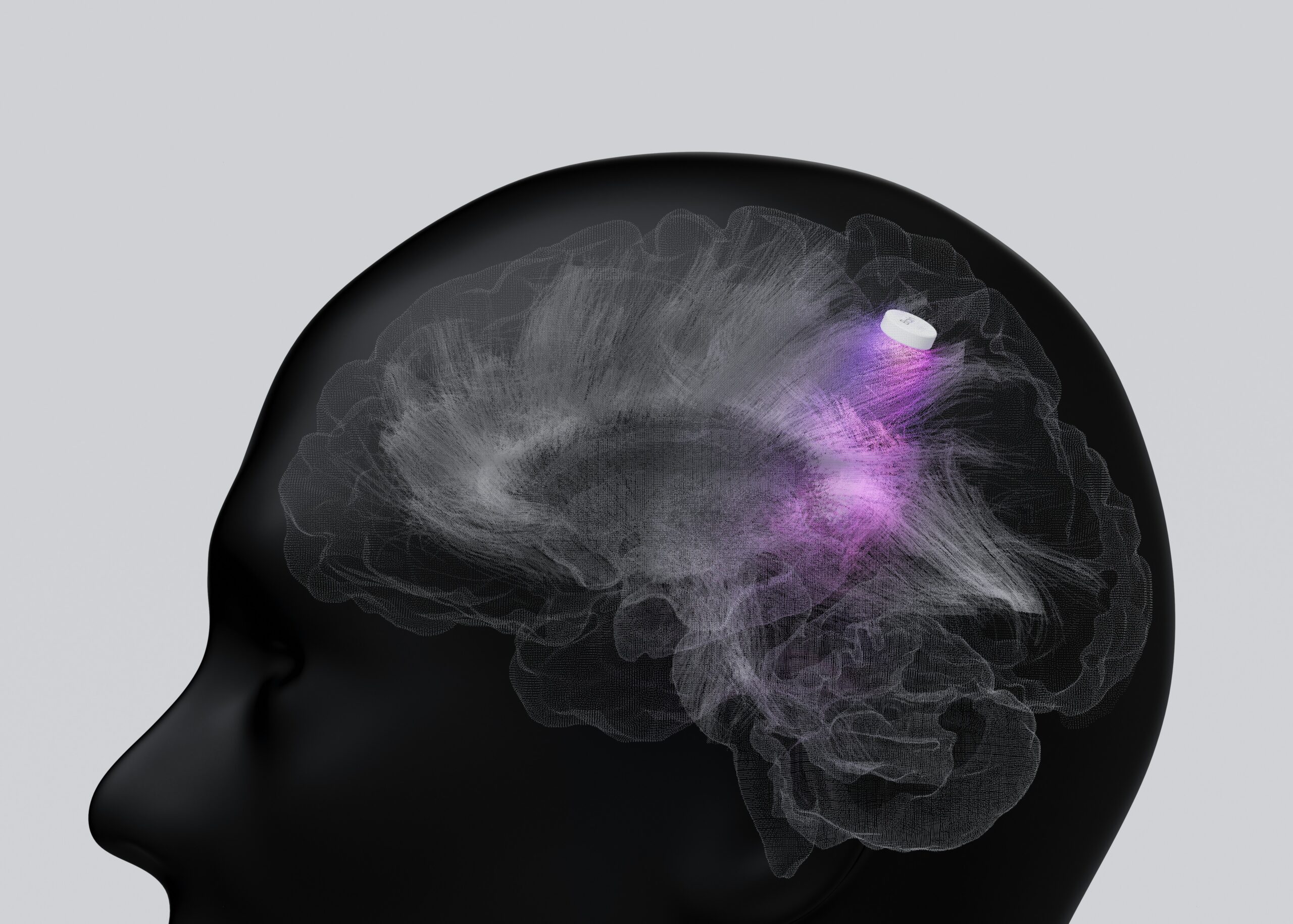
In a typical brain, eating food activates the reward system, which helps reinforce nourishing behaviors and contributes to feelings of satisfaction. Activity in particular brain regions, such as the amygdala and ventral striatum, has been associated with reward anticipation, suggesting that anorexia may involve altered neural responses not only to eating, but to the expectation of eating.
Instead of experiencing pleasure from food, the brain may become conditioned to associate restriction with relief or achievement. This neurological shift makes it easier to continue restricting, even when the body is clearly undernourished, as the brain begins to misinterpret self-denial as rewarding. Over time, the natural cues and reinforcements tied to hunger and satisfaction may begin to fade, reducing interoceptive awareness and making it harder to respond appropriately to internal signals of need.
3. It Causes Structural Changes to the Brain
Malnutrition doesn’t just disrupt brain chemistry; it can also affect the brain’s physical structure. One of the more well-documented consequences of anorexia is the loss of grey matter, particularly in regions involved in cognition and emotional regulation.
Grey matter plays a critical role in essential functions such as emotional processing, memory consolidation, motor coordination, and executive functioning. Neuroimaging studies have shown that individuals with active anorexia often exhibit widespread reductions in grey matter volume, including the frontal, temporal, and parietal lobes. These deficits are associated with both the severity and duration of malnutrition. While weight restoration can lead to partial recovery of grey matter volume, full normalization may be limited or delayed without sustained nutritional rehabilitation and comprehensive care.
4. It Alters Personality and Behavior
It’s not uncommon for family members or friends to describe a loved one with anorexia as “not themselves.” They may seem withdrawn or disconnected in ways that feel unfamiliar or difficult to explain.
This change often reflects disruptions in the brain’s emotional processing systems. Research has shown increased activity in the amygdala in individuals with anorexia, which may contribute to heightened sensitivity to emotional stimuli and difficulty regulating responses. At the same time, many people with anorexia experience alexithymia, which is a reduced ability to identify or describe their own emotions. They may appear emotionally distant, and there can be an impact on inhibition. These traits can make it harder to connect with others or respond flexibly in social situations.
Many describe the experience as having two internal voices: their own, and the eating disorder voice that overrides it. That voice can be persuasive and persistent, making it harder to act in alignment with recovery even when the desire to heal is present.
A Brain That Can Heal
Understanding how anorexia alters the brain offers clarity about what recovery truly requires. Malnutrition affects not just physical health but how a person thinks, feels, and responds. Emotional signals may be misinterpreted or blocked and motivation can become misdirected. The ability to reflect or connect may feel out of reach, not due to lack of effort, but because of real neurological shifts.
Reversing these changes takes time. The brain needs consistent nourishment to begin repairing itself, so that the structures responsible for decision-making, memory, and emotional integration can regain function. The good news is that cognitive flexibility will improve, and patterns that once felt automatic will begin to loosen. Some individuals describe moments of clarity returning as their thoughts grow quieter and more expansive.
Support plays a critical role in this process. When someone resists help or seems ambivalent about recovery, it may reflect the state of their brain more than a fixed mindset. Encouraging nourishment isn’t just about symptom management. It’s a way of helping the person regain access to the parts of themselves that have been overshadowed.
Healing unfolds slowly. It’s not about compliance or willpower. It’s about restoring the conditions that allow a person to reconnect with their body, their thoughts, and the people around them.
Clinically Reviewed By

Nick Kahm, PhD
Co-Founder
Nick Kahm, a former philosophy faculty member at St. Michael's College in Colchester, VT, transitioned from academia to running the Kahm Clinic with his mother. He started the clinic to train dietitians in using Metabolic Testing and Body Composition Analysis for helping people with eating disorders. Now, he is enthusiastic about expanding eating disorder treatment through the Kahm Center for Eating Disorders in Vermont.